The report on the infected blood scandal lays bare “decades of gross and culpable failures”, according to a law firm which represented hundreds of Scots affected by contaminated blood.
Thompsons Solicitors, which represented 300 individuals and two charities in the Infected Blood Inquiry, said the “hard-hitting” report set out a number of Scotland-specific failures that led to “so much suffering and death”.
These included, the firm said, failures in Scottish blood transfusion services in the 1980s and numerous “missed opportunities” to remedy the injustices brought about by the scandal.
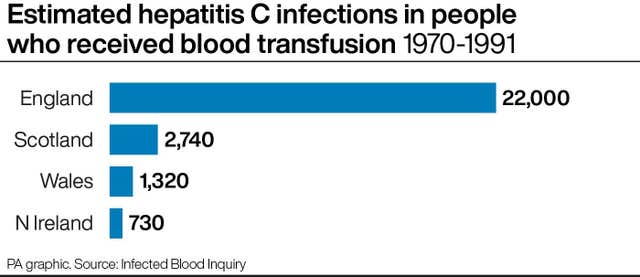
The infected blood scandal saw thousands of patients becoming infected with HIV and hepatitis C after being given contaminated blood products in the 1970s and 1980s, with around 2,400 people dying.
It is estimated that around 3,000 people in Scotland were given contaminated blood, whether through NHS transfusions or as part of haemophilia treatment, with hundreds subsequently dying.
Lynn Carey, associate at Thompsons, said: “We welcome the publication of the report on behalf of every Scottish victim of the contaminated blood scandal. The report is hard-hitting and in many ways difficult to read.
“Sir Brian Langstaff has laid bare the decades of gross and culpable failures that caused so much pain, suffering and death.”
The report found what Ms Carey described as “significant failings” in Scotland, including poor facilities and inadequate staffing at regional transfusion centres, a failure to introduce testing and what she called “culpable” failures at the Protein Fractionation Centre (PFC).
The PFC in Edinburgh was set up in the 1970s in order to produce blood products for use in Scotland and the north of England, but was never used for this purpose.
The report found that this contributed to a failure to supply enough Factor VIII plasma from UK donors to meet foreseeable demand, leading to a need to import plasma from abroad.
The report was also critical of decisions at Yorkhill hospital in Glasgow that saw children suffering from haemophilia receive plasma products sourced from paid donors in the United States, despite these being known to be high risk.
In all, 21 children become infected with HIV at the hospital.
The report attributed this to decisions taken by the-then centre director Dr Michael Willoughby, saying: “It makes little sense for Dr Willoughby to have committed Yorkhill to the purchase of commercial concentrates when throughout the period of interest Scotland was effectively self-sufficient in NHS factor concentrates.”
The report also set out that since the scandal there had been “a series of missed opportunities to remedy (in small measure at least) the injustices that had been, and continued to be, experienced.”
It listed a number of missed opportunities, including an investigation by the Scottish Executive, recommendations from the Health and Care Committee and the recommendations of an expert group appointed by the Scottish Executive, none of which, it says, were taken, resulting instead in the harm being “compounded”.
Ms Carey held up the Penrose Inquiry as a particularly prominent missed opportunity, in the eyes of victims of the scandal.
The Penrose Inquiry into infection from NHS treatment in Scotland with blood and blood products was set up by the Scottish Government in 2008 and issued its final report in 2015.

Ms Carey said: “The victims that we represent all talk of the many missed opportunities over the years for the truth to be found and justice served. We also talk about how the harms of the scandal were compounded by secrecy, cover-up and those missed opportunities.
“The Scottish victims hold the Penrose Report as a missed opportunity that compounded their harms. We have spoken of righting the wrongs of Penrose. Today that wrong has been righted and victims and their families are vindicated.”
Joyce Donnelly, from the Scottish Infected Blood Forum, a charity that supports victims of contaminated blood products in Scotland, said: “The mantra that the government used to trot out about ‘they received the best possible treatment available at the time’ has now proved to be a lie.”
John Dearden, of the charity Haemophilia Scotland, said that in the report Sir Brian had “got to the root of what has been happening over many years”.
He added: “He has made some very astute recommendations and we look forward to the Government responding to us in a positive way.”
Scottish Government public health minister Jenni Minto said: “Today is about those who have been infected, their families and support organisations, and I want to pay tribute to them. They have been focused on ensuring the impact of this terrible tragedy, their suffering, has not been ignored.
“On behalf of the Scottish Government, I reiterate our sincere apology to those who have been infected or affected by NHS blood or blood products.
“The Scottish Government has already accepted the moral case for compensation for infected blood victims and is committed to working with the UK Government to ensure any compensation scheme works as well as possible for victims.
“We are determined to use the inquiry’s report to ensure lessons have been learned so a tragedy like this can never happen again.”
Scottish Conservative leader Douglas Ross said: “This is a momentous day for campaigners who have fought tirelessly for justice and have been wholly vindicated by this devastating report.”
Scottish Labour health spokeswoman Jackie Baillie said: “My thoughts and those of the entire Scottish Labour Party are with all of those who have been affected by this scandal – including those still living with the consequences today.”
NHS Scotland Health Boards said in a statement: “We sincerely apologise for the historical failings described in the Infected Blood Inquiry and empathise with the impact these events had on infected and affected people.
“We welcome the publication of this inquiry and we would like to thank the chair and staff for the work undertaken to produce this comprehensive report.
“Modern safety standards are rigorous and significant advancements in screening and testing protocols have been made since the events that have been the subject of this inquiry. All donated blood then undergoes thorough testing before being used for transfusions.
“NHS Scotland is committed to ensuring lessons from these events have been learned as we continue to prioritise a safe and sustainable blood supply across Scotland.”




Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules here